Review Article |
|
Corresponding author: Irma Melyani Puspitasari ( irma.melyani@unpad.ac.id ) Academic editor: Guenka Petrova
© 2023 Shannon Maidelaine Prijadi, Clara Fernanda Kusuma, Irma Melyani Puspitasari.
This is an open access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation:
Prijadi SM, Kusuma CF, Puspitasari IM (2023) The association between Vitamin D levels and postpartum depression: a review. Pharmacia 70(1): 21-26. https://doi.org/10.3897/pharmacia.70.e97300
|
Abstract
According to WHO, Postpartum Depression (PPD) occurs in 10–15% of women after giving birth. Several studies assumed that vitamin D deficiency might worsen PPD symptoms. However, the association between vitamin D levels and PPD is still conflicting. This article summarizes the association between vitamin D levels and PPD. A literature search about Vitamin D levels and PPD from Scopus and PubMed databases was performed in June 2022. Eleven studies were obtained out of 30 studies. Nine out of 11 studies showed that vitamin D levels were significantly associated with PPD. However, the two others showed no significant association. The difference in the blood sample taken and how to assess depression contributes to a different result. The association is related to the role of vitamin D in mood regulation, synthesis of neurotransmitters, stimulating brain receptors, and intercellular neuronal signaling systems.
Keywords
Postpartum depression, Vitamin D, Pregnancy, Deficiency
Introduction
Postpartum depression (PPD) occurs in women after giving birth with characteristics such as weakness, feelings of guilt, unable to sleep, decreased cognitive function, and feelings of suicide. Generally, postpartum depression symptoms appear 3–6 months after birth (
Vitamin D is a fat-soluble vitamin usually found naturally in food, sunlight, and supplements. Sources of vitamin D come from food, such as fish oil, red meat, liver, egg yolks, and cow’s milk (
The association between vitamin D levels and PPD is still conflicting. Several studies assumed that vitamin D deficiency might worsen PPD symptoms (
Methods
Data search
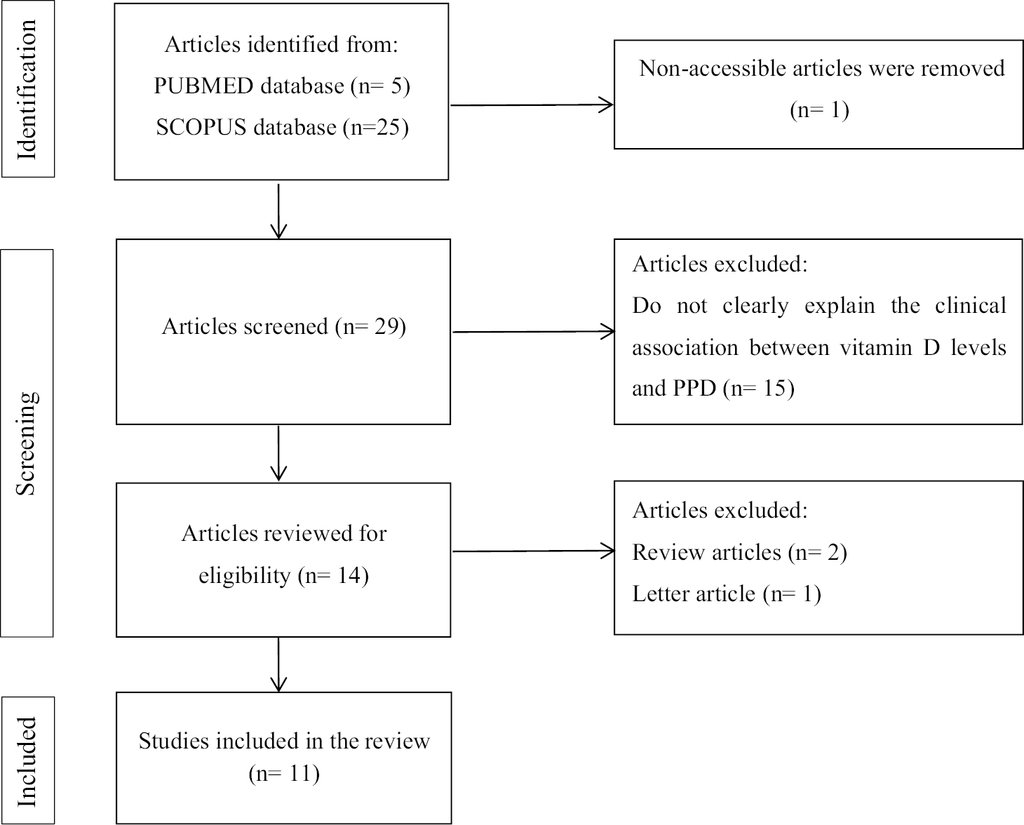
In June 2022, a literature search was conducted using the PUBMED and SCOPUS databases. “Vitamin D” and “postpartum depression” were the keywords used. The flow diagram’s literature search report adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Study selection
Original research articles in English published between 2012 and 2022 are eligible for inclusion. Articles that did not discuss the relationship between vitamin D and PPD were not considered.
Article extraction
The author’s name, type of study, country, number of participants, age, depression test, methods for measuring the vitamin D levels, study objective, type of sample, time for taking the samples, time for depression assessment, levels of vitamin D, depression scale score, and conclusion were extracted from the obtained articles.
Result and discussion
Fig.
Table
Studies of the relationship between Vitamin D and post-partum depression.
| No. | Authors | Type of Study | Country | Number of Participants | Age | Depression test | Vit D measurement methods |
|---|---|---|---|---|---|---|---|
| 1 | Pillai, R. R., et al | Cross-sectional study | South India | 660 | 18–40 | EPDS | ELISA |
| 2 | Abedi, P., et al | Case-control | Iran | 120 | 18–35 | BDS | ELISA |
| 3 | Nielsen, N. O, et al | Case-control | Denmark | Case = 605 Control = 875 | 18–34+ | Taking anti-depressant within one year after delivery | LCMS/ MS |
| 4 | Gould J. F, et al | Randomized controlled trial | Australia | 1040 | 24–35 | EPDS | LCMS/ MS |
| 5 | Amini S, et al | Randomized controlled trial | Iran | 81 | 18–45 | EPDS | ELISA |
| 6 | Rouhi, M., et al | Randomized controlled trial | Iran | 80 | Mean: 24.7 | EPDS | - |
| 7 | Accortt, E. E, et al (2015) | Cohort study | USA | 91 | 18–44 | CES-D and EPDS | A competitive chemiluminescence immunoassay |
| 8 | Accortt, E. E, et al (2020) | Cohort study | USA | 89 | average 27.80 | BDI and CES-D | Reverse-phase liquid chromatography |
| 9 | Fu, C. et al | Cohort study | China | 248 | Median: 31 (29–32) | EPDS | E601 modular analyzer |
| 10 | Gur, EB, et al | Cohort study | Turkey | 208 | 18–40 | EPDS | ELISA |
| 11 | Robinson, M., et al | Cohort study | Australia | 796 | <20–>30 | EPDS | Enzyme immunoassay |
| Total = 4,893 | |||||||
Studies with a significant association between vitamin D levels and PPD
Table
| Study No | Authors | Study objective | Sample | The sample was taken at | Depression assessment | Level of Vit D | Depression scale score | Conclusion |
|---|---|---|---|---|---|---|---|---|
| 1. | Pillai, R. R., et al | To compare serum 25(OH)D concentrations in women with and without PPD. | 5 ml of peripheral venous blood | 6 weeks post delivery | at 6 weeks post delivery | Total Vit D With PPD: 23 (18.1–28.6) Without PPD: 26 (18.2–34.9) | With PDD: 13 (11–15) Without PDD: 3 (1–6) | Low 25(OH)D serum levels are associated with depression in women 6 weeks after delivery. |
| 2 | Abedi, P., et al | To investigate the association between vitamin D and postpartum depression in Iranian women of reproductive age. | 5mL venous blood | at 6–8 weeks after childbirth. | at 6–8 weeks after birth. | With PPD: 16.89±7.05 Without PPD: 21.28±7.13 | - | There is an association between low vitamin D levels and postpartum depression in Iranian women of reproductive age. |
| 5. | Amini S, et al | To see how vitamin D and calcium supplementation affected the severity of symptoms and some inflammatory biomarkers in women with PPD. | 5 ml of fasting blood samples were collected pre-and post-intervention. | at baseline and the end of the study. | at baseline and the end of the study | Vit D+Ca: Baseline: 36.56 (28.67, 46.72) Post-intervention: 51.39 (39.73, 63.04) p = 0.003 Vit D+Ca placebo: Baseline: 39.83 (31.94, 47.69) Post-intervention: 58.03 (45.17, 70.91) p < 0.001 Placebo: Baseline: 36.74 (28.40, 45.05) Post-intervention: 42.90 (33.77, 52.04) p = 0.025 | Vit D+Ca: Baseline: 17.41 (4.10) Post-intervention: 15.70 (5.15) p = 0.042 Vit D+Ca placebo: Baseline: 17.50 (3.97) Post-intervention: 13.33 (6.38) p = 0.004 Placebo: Baseline: 16.43 (3.07) Post-intervention: 16.68 (5.99) p = 0.586 | Vitamin D supplementation with an oral pill containing 50,000 IU vitamin D3 fortnightly for 8 weeks improved PPD symptoms and serum 25[OH]D concentrations. |
| 6. | Rouhi, M., et al | To assess the effectiveness of vitamin D supplements in treating postnatal depression and fatigue. | Vitamin D deficiency was not assessed by blood samples. | - | at baseline and end of the study (six months after the study) | - | Baseline: Vit D group: 15.1 (1.9) Placebo group: 15.3 (1.8) Post-intervention: Vit D group: 8.6 (4.3) Placebo group: 13.4 (4.7) | Vitamin D reduced depression and fatigue in the intervention group (P < 0.001). |
| 7. | Accortt, E. E, et al | To see if low prenatal vitamin D status predicted PPD symptoms in pregnant African-American women. | a 10–ml blood | the second-trimester research visit (13–28 weeks gestation). | routine postpartum visits, which are usually scheduled 4–6 weeks after delivery | 13.2±9.4 | Prenatal CES-D:16.1±11 EPDS 5.20±4.95 | In African American women, low prenatal 25(OH)D and high prenatal inflammation may predict future postpartum depressive symptoms. |
| 8. | Accortt, EE, et al | To investigate the relationship between the Vitamin D Metabolite Ratio (VMR), a new candidate biomarker during pregnancy, and PPD. | Plasma | in the second trimester (18–20 weeks gestation) | in the third trimester (28–30 weeks gestation) using BDI; at 6–10 weeks postpartum with CESD | Not at PPD risk: 30 (50.8) PPD risk: 17 (56.7) | Prenatal BDI: Not at PPD risk: 12.4 PPD risk: 14.9 Postpartum CES-D Not at PPD risk: 8.7 PPD risk: 22.0 | Vitamin D deficiency, as measured by the VMR, is associated to an increased risk of PPD. |
| 9. | Fu, C. W. et al | To investigate the possible association between serum 25[OH]D (25-hydroxyvitamin D) levels collected 24 hours after delivery and postpartum depression in a Chinese cohort sample. | blood | A blood sample was taken between 24 and 48 hours after the birth. | within 3 months after delivery | Serum 25 [OH]D levels were significantly higher in women without PPD than in women with PPD [14.3 (IQR 10.2–18.2) versus 8.3 (IQR 7.5–9.3) ng/ml; P 0.0001. | At three months’ follow-up, 26 women (12.2%) were identified with PPD. | lower serum 25[OH]D levels were associated with postpartum depression. |
| 10. | Gur, E.B., et al | To investigate a possible association between PPD and serum levels of 25-hydroxy vitamin D3 (25 (OH)D3) during mid-pregnancy. | blood | Between 24–28 weeks of pregnancy | 1 week, 6 week, and 6 month after delivery | Average 22.4 (11.2) | 1st week Postpartum: 17.6 6th weeks Postpartum 18.9 6th months Postpartum 16.6 | Vitamin D levels during pregnancy may be associated to an increase in depressive symptoms in postpartum women. |
| 11. | Robinson, M., et al | To assess mid-pregnancy women’s 25(OH)D levels in relation to PPD | Venous blood | at 18 weeks of pregnancy | 3 days after delivery | - | - | A lower level of 25(OH)-vitamin D in serum at 18 week gestation was associated to an increased risk of postnatal depression symptoms three days after birth. |
A cross-sectional study in South India that measured serum 25(OH)D levels in women with and without PPD discovered that low serum 25(OH)D levels are associated with depression in women six weeks after delivery (
Vitamin D supplementation had positive effects on PPD symptoms and serum concentrations of 25[OH]D, according to two randomized controlled trials by
Five cohort studies conducted in the USA, China, Turkey, and Australia revealed that low vitamin D levels during pregnancy and childbirth were associated with PPD. In the United States, Accortt et al. reported that low prenatal 25(OH)D and high prenatal inflammation may predict future postpartum depressive symptomatology in African American women, and Vitamin D deficiency, as measured by the Vitamin D Metabolite Ratio (VMR), is associated with an increased risk of PPD (
Studies with no significant association between Vitamin D levels and PPD
Table
| Study No | Authors | Study objective | Sample | The sample was taken at | Depression assessment | Level of Vit D | Depression scale score | Conclusion |
|---|---|---|---|---|---|---|---|---|
| 3. | Nielsen, N. O, et al | To determine if low vitamin D levels during pregnancy are associated with a higher risk of PPD. | Venous blood on routine visits | Weeks 25 pregnancy | Taking anti-depressant within one year after delivery | With PPD: 55.62 nmol/L Without PPD: 55.60 nmol/L | - | There was no overall relationship between vitamin D status during pregnancy and PPD risk. |
| 4. | Gould J. F, et al | To investigate the relationship between 25(OH)D at birth and the risk of PPD six weeks and six months later in a large cohort of Australian women. | Cord blood sample | at delivery | six weeks and six months after birth | Over half of the women (58%, n = 598) had cord blood 25(OH)D > 50 nmol/L, 34% (n = 358) had 25(OH)D 25–50 nmol/L, and 8% (n = 84) had 25(OH)D 25 nmol/L. | - | There was no association found between cord blood 25(OH)D concentration at delivery and PPD six weeks or six months later. |
Association between Vitamin D levels and PPD
Our study revealed that most studies (9 out of 11) of Vitamin D levels were associated with PPD. A theory suggests that vitamin D plays an important role in mood regulation. Mood regulation and the incidence of depression are closely related to neurotransmitters. The association of low vitamin D levels with depression is related to hypothalamic function and neurotransmitter production (
Vitamin D deficiency has been proposed to contribute to brain development and function in humans based on animal studies (
Conclusion
Most studies found a significant association between vitamin D levels and PPD. The association is related to the role of vitamin D in mood regulation, influencing the synthesis of neurotransmitters, stimulating receptors in the brain, and being involved in the intercellular neuronal signaling system.
Funding
Universitas Padjadjaran Indonesia supports this work.
Disclosure
The authors have declared no conflicts of interest in this work.
References
- Abedi P, Bovayri M, Fakhri A, Jahanfar S (2018) The relationship between Vitamin D and postpartum depression in reproductive-aged iranian women. Journal of Medicine and Life 11: 286–292. https://doi.org/10.25122/jml-2018-0038
- Accortt EE, Schetter CD, Peters RM, Cassidy-Bushrow AE (2016) Lower prenatal vitamin D status and postpartum depressive symptomatology in African American women: Preliminary evidence for moderation by inflammatory cytokines. Archives of Women’s Mental Health 19: 373–383. https://doi.org/10.1007/s00737-015-0585-1
- Accortt EE, Arora C, Mirocha J, Jackman S, Liang R, Karumanchi SA, Berg AH, Hobel CJ (2021) Low prenatal Vitamin D metabolite ratio and subsequent postpartum depression risk. Journal of Women’s Health 30: 113–120. https://doi.org/10.1089/jwh.2019.8209
- Akpınar Ş, Karadağ MG (2022) Is Vitamin D important in anxiety or depression? What is the truth? Current Nutrition Reports 11: 675–681. https://doi.org/10.1007/s13668-022-00441-0
- Amini S, Jafarirad S, Amani R (2019) Postpartum depression and vitamin D: A systematic review. Critical Reviews in Food Science and Nutrition 59: 1514–1520. https://doi.org/10.1080/10408398.2017.1423276
- Amini S, Amani R, Jafarirad S, Cheraghian B, Sayyah M, Hemmati AA (2022) The effect of vitamin D and calcium supplementation on inflammatory biomarkers, estradiol levels and severity of symptoms in women with postpartum depression: a randomized double-blind clinical trial. Nutritional Neuroscience 25: 22–32. https://doi.org/10.1080/1028415X.2019.1707396
- Berridge MJ (2017) Vitamin D and depression: Cellular and regulatory mechanisms. Pharmacological Reviews 69: 80–92. https://doi.org/10.1124/PR.116.013227
- CDC (2014) Depression is Not a Normal Part of Growing Older. Centers of Disease Control and Prevention. https://www.cdc.gov/aging/depression/index.html#:~:text%=%Depression%20is%20a%20true%20and,to%20be%20diagnosed%20and%20treated [July 31, 2022]
- Ellsworth-Bowers ER, Corwin EJ (2012) Nutrition and the psychoneuroimmunology of postpartum depression. Nutrition Research Reviews 25: 180–192. https://doi.org/10.1017/S0954422412000091
- Fu CW, Liu JT, Tu WJ, Yang JQ, Cao Y (2015) Association between serum 25-hydroxyvitamin D levels measured 24 hours after delivery and postpartum depression. BJOG: An International Journal of Obstetrics and Gynaecology 122: 1688–1694. https://doi.org/10.1111/1471-0528.13111
- Geng C, Shaikh AS, Han W, Chen D, Guo Y, Jiang P (2019) Vitamin D and depression: mechanisms, determination and application. Asia Pacific Journal of Clinical Nutrition 28: 689–694. https://doi.org/10.6133/apjcn.201912_28(4).0003
- Gould JF, Anderson AJ, Yelland LN, Smithers LG, Skeaff CM, Gibson RA, Makrides M (2015) Association of cord blood Vitamin D at delivery with postpartum depression in Australian women. Australian and New Zealand Journal of Obstetrics and Gynaecology 55: 446–452. https://doi.org/10.1111/ajo.12344
- Gur EB, Gokduman A, Turan GA, Tatar S, Hepyilmaz I, Zengin EB, Eskicioglu F, Guclu S (2014) Mid-pregnancy vitamin D levels and postpartum depression. European Journal of Obstetrics and Gynecology and Reproductive Biology 179: 110–116. https://doi.org/10.1016/j.ejogrb.2014.05.017
- Khan B, Shafiq H, Abbas S, Jabeen S, Khan SA, Afsar T, Almajwal A, Alruwaili NW, al-disi D, Alenezi S, Parveen Z, Razak S (2022) Vitamin D status and its correlation to depression. Annals of General Psychiatry 21: 32. [9 pp] https://doi.org/10.1186/s12991-022-00406-1
- Menon V, Kar SK, Suthar N, Nebhinani N (2020) Vitamin D and depression: A critical appraisal of the evidence and future directions. Indian Journal of Psychological Medicine 42: 11–21. https://doi.org/10.4103/IJPSYM.IJPSYM_160_19
- NHS Choices (2017) Vitamin D - NHS Choices. NHS Choices. [Available from:] https://www.nhs.uk/conditions/vitamins-and-minerals/vitamin-d/ [August 1, 2022]
- Nielsen NO, Strøm M, Boyd HA, Andersen EW, Wohlfahrt J, Lundqvist M, Cohen A, Hougaard DM, Melbye M (2013) Vitamin D status during pregnancy and the risk of subsequent postpartum depression: A case-control study. PLoS ONE 8(11): e80686. https://doi.org/10.1371/journal.pone.0080686
- Pet MA, Brouwer-Brolsma EM (2016) The Impact of Maternal Vitamin D status on offspring brain development and function: a systematic review. Advances in Nutrition 7: 665–678. https://doi.org/10.3945/an.115.010330
- Pillai RR, Premkumar NR, Kattimani S, Sagili H, Wilson AB, Sharon L, Rajendiran S (2021) Reduced maternal serum total, free and bioavailable Vitamin D levels and its association with the risk for postpartum depressive symptoms. Archives of Medical Research 52: 84–92. https://doi.org/10.1016/j.arcmed.2020.10.003
- Robinson M, Whitehouse AJO, Newnham JP, Gorman S, Jacoby P, Holt BJ, Serralha M, Tearne JE, Holt PG, Hart PH, Kusel MMH (2014) Low maternal serum vitamin D during pregnancy and the risk for postpartum depression symptoms. Archives of Women’s Mental Health 17: 213–219. https://doi.org/10.1007/s00737-014-0422-y
- Rouhi M, Rouhi N, Mohamadpour S, Tajrishi HPR (2018) Vitamin D reduces postpartum depression and fatigue among Iranian women. 26: 787–793. https://doi.org/10.12968/BJOM.2018.26.12.787
- WHO (2012) Health topics: Depression. Depression. https://www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health?gclid=Cj0KCQjw08aYBhDlARIsAA_gb0egywsrxfy_ZGqZ5CIMPh087UkTVKdpvjww3NVE9oM3bBdAXooFZzYaAntrEALw_wcB [July 30, 2022]